Αντιπροσωπείες
Η Getremed παρέχει πλήρεις και αξιόπιστες λύσεις στον ΩΡΛ χώρο από το 1985. Με άρτια επιστημονική γνώση και τεχνογνωσία, καλύπτουμε με αφοσίωση όλο το φάσμα των αναγκών της συγχρονης Ωτορινολαρυγγολογίας και Νευροχειρουργικής, από τον εξοπλισμό ιατρείου, μέχρι τις εξειδικευμένες συσκευές, εργαλεία, αναλώσιμα και εμφυτεύματα υψηλής τεχνολογίας του χειρουργείου.






Ιατρικά προϊόντα
Με κορυφαίες αντιπροσωπείες η Getremed προσφέρει ολοκληρωμένες λύσεις για Χειρουργεία, Ιατρεία και Φροντίδα στο σπίτι.
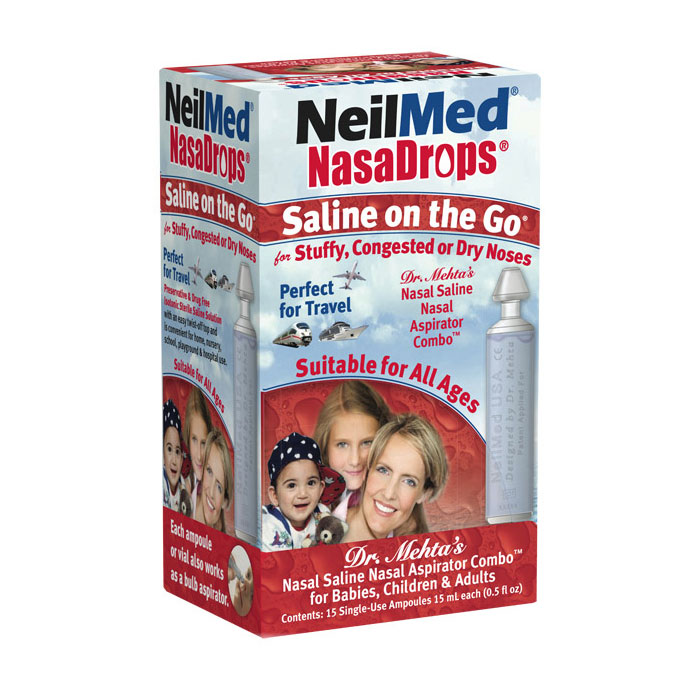
Προϊόντα Φαρμακείου
Αξιόπιστες λύσεις για ενήλικες και παιδιά
Προσφορές
Δείτε τις προσφορές μας και κερδίστε!